The Health Resources and Services Administration’s Maternal and Child Health Bureau (MCHB) recently released a Blueprint for Change: A National Framework for a System of Services for Children and Youth with Special Health Care Needs. The document serves as a national agenda and framework to advance the system that serves children and youth with special health care needs (CYSHCN) to improve their lives and well-being. MCHB defines a child or youth with a special health care need as “those who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally.”
MCHB partnered with families, family-run organizations, health care professionals and public health leaders to create the Blueprint. Together, they built the Blueprint on these principles:
- families are partners in decision-making;
- medical home access;
- early and continuous screening for special health care needs (operationalized through receipt of preventive health care);
- continuous and adequate health insurance;
- access to community-based services; and
- for children ages 12 to 17 years, receipt of healthcare transition planning services.
The Blueprint stresses that children and youth with special health care needs should “enjoy a full life, from childhood through adulthood, and thrive in a system that supports their social, health, and emotional needs, ensuring dignity, autonomy, independence, and active participation in their communities.”
These are the assumptions that underlie the Blueprint for Change’s principles and strategies:
- “Disability is a natural part of the human experience and in no way diminishes the right of individuals to participate in or contribute to society.”
- “Racism is a social risk factor that has a profound impact on the health status of children, adolescents, young adults, and their families.”
- “CYSHCN require more and different types of services than those for typically developing children and youth, yet the current system is not ensuring access to these services, particularly for CYSHCN impacted by poverty and discrimination.”
- “CYSHCN are more severely impacted by the adverse effects of social determinants of health and inequities.”
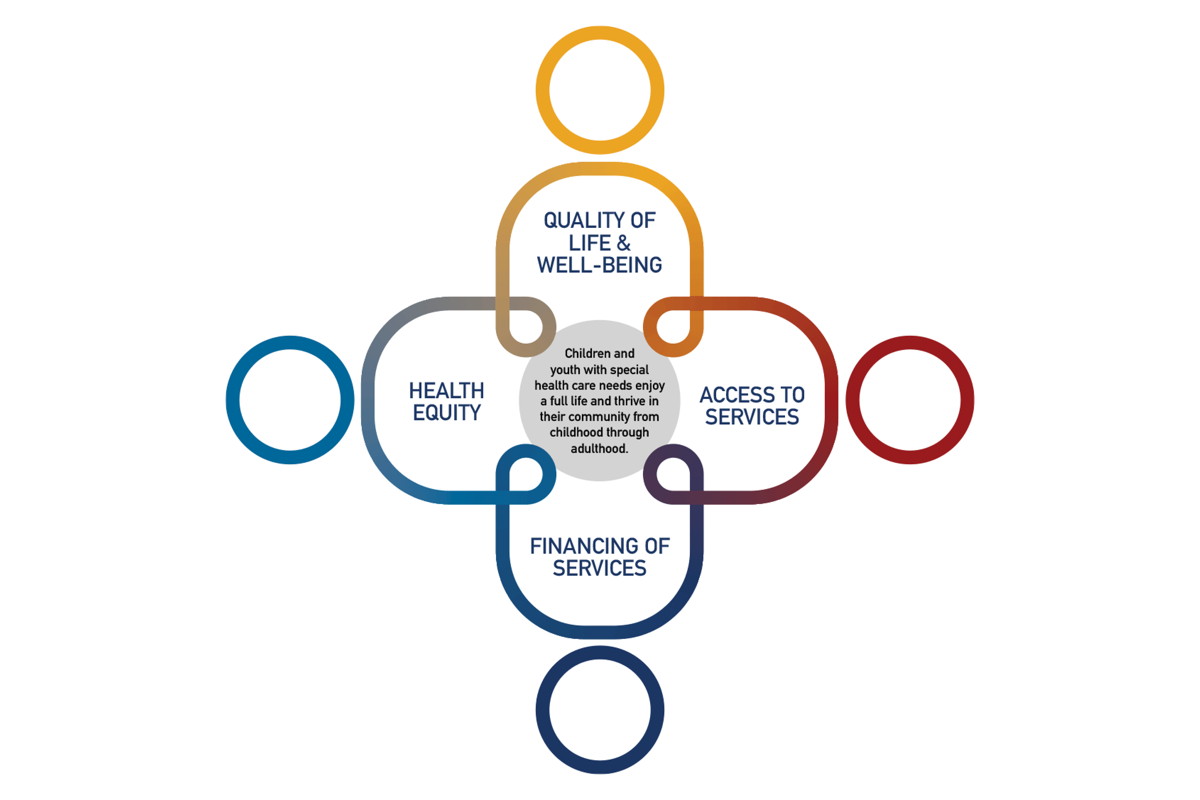
The Blueprint addresses critical areas of need and outlines a vision for change and guiding principles under each one. The areas of need, visions and principles are quoted verbatim.
Critical Area 1: Health Equity
Vision: All CYSHCN have a fair and just opportunity to be as healthy as possible and thrive throughout their lives (e.g., from school to the workforce) without discrimination and regardless of the circumstances in which they were born or live.
Principle 1: Structural and systemic causal barriers to health equity are eliminated, including discrimination, poverty, and other social risk factors.
Principle 2: Sectors, systems, and programs that fund, deliver, and monitor services and supports for CYSHCN are designed and implemented to reduce health disparities and improve health outcomes for all CYSHCN.
Critical Area 2: Family and Child Well-Being and Quality of Life
Vision: The service system prioritizes quality of life, well-being and supports flourishing for CYSHCN and their families.
Principle 1: Families, regardless of circumstance, can access high-quality, affordable, community-based services that support the medical, behavioral, social, and emotional well-being of the child or youth and whole family.
Principle 2: Health systems place value on the measurement and use of both child and family well-being and quality-of-life outcomes, and health outcomes.
Critical Area 3: Access to Services
Vision: CYSHCN and their families have timely access to the integrated, easy-to-navigate, high-quality health care and supports they need, including but not limited to physical, oral, and behavioral health providers; home and community-based supports; and care coordination throughout the life course. This critical area recognizes the educational system as an entry point and major deliverer of services for children and families.
Principle 1: All services and supports at the individual, family, community, and provider levels are easy for families and professionals to navigate when, where, and how they need them.
Principle 2: The workforce is trained to meet the needs of CYSHCN and their families, reflects the families and communities they serve, and is culturally responsive.
Principle 3: Service sectors increase the ability of CYSHCN and their families to access services by addressing administrative and other processes that hinder access
Critical Area 4: Financing of Services
Vision: Health care and other related services are accessible, affordable, comprehensive, and continuous; they prioritize the well-being of CYSHCN and families.
Principle 1: Health care and other related services for CYSHCN and families are financed and paid for in ways that support and maximize an individual’s values and choice in meeting needs.
Principle 2: Health and social service sector investments address social determinants of health to increase family well-being and flourishing.
Principle 3: Payers and service sectors adopt value-based payment strategies that support families, advance equity, and incorporate continuous quality improvement by enhancing team-based integrated ca
The Blueprint goes on to say that the Bureau has learned, through both successes and challenges, several key lessons:
- “we must engage families meaningfully through all steps of the process;”
- “to strengthen the system of services for CYSHCN, we must be able to define and measure the population and components of the system;”
- “we must continually assess and evaluate the Bureau’s research and programmatic resources to address ongoing and emerging issues that impact CYSHCN and the services they receive;”
- “we must always approach this work through a lens of equity; and”
- “MCHB has a unique and enduring role as the only federal agency with a statutory responsibility to support systems of care for CYSHCN.”
The plan also states: “As the US health care system strives to reach the health care goals of safe, efficient, effective, equitable, timely, and patient-centered care, youth and families must be equal partners at all levels of the health care system—from clinical decision making to designing and implementing programs and policies…. access to services should start based on where and how families desire services and supports that prioritize family health and wellness. Access to services for CYSHCN should openly address equity and cultural humility. For maximum effectiveness of service delivery, cultural humility should be the design underpinning, not a programmatic addition. The workforce ideally should reflect the community and be aligned with family goals for coordination of care and quality of life.”
Families as Allies is excited about this Blueprint because it’s consistent with our mission that families are partners in their children’s care. By that, we mean that Mississippi’s system of care for children must be family-driven. We look forward to working with families, providers, the community, policymakers and state and local systems to make this Blueprint a reality in Mississippi. We especially appreciate our partnership with the Missississippi State Department of Health and the Department’s commitment to family-centered practice and the principles in the Blueprint.
If you have ideas about how Mississippi stakeholders can implement this Blueprint or if you have questions or concerns about your child with special health care needs, please feel free to reach out to us. We want to work together.
[Image courtesy MCHB]